-
Faculty of Arts and HumanitiesDean's Office, Faculty of Arts and HumanitiesJakobi 2, r 116-121 51005 Tartu linn, Tartu linn, Tartumaa EST0Institute of History and ArchaeologyJakobi 2 51005 Tartu linn, Tartu linn, Tartumaa EST0Institute of Estonian and General LinguisticsJakobi 2, IV korrus 51005 Tartu linn, Tartu linn, Tartumaa EST0Institute of Philosophy and SemioticsJakobi 2, III korrus, ruumid 302-337 51005 Tartu linn, Tartu linn, Tartumaa EST0Institute of Cultural ResearchÜlikooli 16 51003 Tartu linn, Tartu linn, Tartumaa EST0Institute of Foreign Languages and CulturesLossi 3 51003 Tartu linn, Tartu linn, Tartumaa EST0School of Theology and Religious StudiesÜlikooli 18 50090 Tartu linn, Tartu linn, Tartumaa EST0Viljandi Culture AcademyPosti 1 71004 Viljandi linn, Viljandimaa EST0Professors emeriti, Faculty of Arts and Humanities0Associate Professors emeriti, Faculty of Arts and Humanities0Faculty of Social SciencesDean's Office, Faculty of Social SciencesLossi 36 51003 Tartu linn, Tartu linn, Tartumaa EST0Institute of EducationJakobi 5 51005 Tartu linn, Tartu linn, Tartumaa EST0Johan Skytte Institute of Political StudiesLossi 36, ruum 301 51003 Tartu linn, Tartu linn, Tartumaa EST0School of Economics and Business AdministrationNarva mnt 18 51009 Tartu linn, Tartu linn, Tartumaa EST0Institute of PsychologyNäituse 2 50409 Tartu linn, Tartu linn, Tartumaa EST0School of LawNäituse 20 - 324 50409 Tartu linn, Tartu linn, Tartumaa EST0Institute of Social StudiesLossi 36 51003 Tartu linn, Tartu linn, Tartumaa EST0Narva CollegeRaekoja plats 2 20307 Narva linn, Ida-Virumaa EST0Pärnu CollegeRingi 35 80012 Pärnu linn, Pärnu linn, Pärnumaa EST0Professors emeriti, Faculty of Social Sciences0Associate Professors emeriti, Faculty of Social Sciences0Faculty of MedicineDean's Office, Faculty of MedicineRavila 19 50411 Tartu linn, Tartu linn, Tartumaa ESTInstitute of Biomedicine and Translational MedicineBiomeedikum, Ravila 19 50411 Tartu linn, Tartu linn, Tartumaa ESTInstitute of PharmacyNooruse 1 50411 Tartu linn, Tartu linn, Tartumaa ESTInstitute of DentistryL. Puusepa 1a 50406 Tartu linn, Tartu linn, Tartumaa ESTInstitute of Clinical MedicineL. Puusepa 8 50406 Tartu linn, Tartu linn, Tartumaa ESTInstitute of Family Medicine and Public HealthRavila 19 50411 Tartu linn, Tartu linn, Tartumaa ESTInstitute of Sport Sciences and PhysiotherapyUjula 4 51008 Tartu linn, Tartu linn, Tartumaa ESTProfessors emeriti, Faculty of Medicine0Associate Professors emeriti, Faculty of Medicine0Faculty of Science and TechnologyDean's Office, Faculty of Science and TechnologyVanemuise 46 - 208 51003 Tartu linn, Tartu linn, Tartumaa ESTInstitute of Computer ScienceNarva mnt 18 51009 Tartu linn, Tartu linn, Tartumaa ESTInstitute of GenomicsRiia 23b/2 51010 Tartu linn, Tartu linn, Tartumaa ESTEstonian Marine Institute0Institute of PhysicsInstitute of ChemistryRavila 14a 50411 Tartu linn, Tartu linn, Tartumaa EST0Institute of Mathematics and StatisticsNarva mnt 18 51009 Tartu linn, Tartu linn, Tartumaa EST0Institute of Molecular and Cell BiologyRiia 23, 23b - 134 51010 Tartu linn, Tartu linn, Tartumaa ESTTartu ObservatoryObservatooriumi 1 61602 Tõravere alevik, Nõo vald, Tartumaa EST0Institute of TechnologyNooruse 1 50411 Tartu linn, Tartu linn, Tartumaa ESTInstitute of Ecology and Earth SciencesJ. Liivi tn 2 50409 Tartu linn, Tartu linn, Tartumaa ESTProfessors emeriti, Faculty of Science and Technology0Associate Professors emeriti, Faculty of Science and Technology0Institute of BioengineeringArea of Academic SecretaryHuman Resources OfficeUppsala 6, Lossi 36 51003 Tartu linn, Tartu linn, Tartumaa EST0Area of Head of FinanceFinance Office0Area of Director of AdministrationInformation Technology Office0Administrative OfficeÜlikooli 17 (III korrus) 51005 Tartu linn, Tartu linn, Tartumaa EST0Estates Office0Marketing and Communication OfficeÜlikooli 18, ruumid 102, 104, 209, 210 50090 Tartu linn, Tartu linn, Tartumaa EST0Area of Vice Rector for DevelopmentCentre for Entrepreneurship and InnovationNarva mnt 18 51009 Tartu linn, Tartu linn, Tartumaa EST0University of Tartu Natural History Museum and Botanical GardenVanemuise 46 51003 Tartu linn, Tartu linn, Tartumaa EST0International Cooperation and Protocol Office0University of Tartu MuseumLossi 25 51003 Tartu linn, Tartu linn, Tartumaa EST0Area of RectorRector's Strategy OfficeInternal Audit OfficeArea of Vice Rector for Academic AffairsOffice of Academic AffairsUniversity of Tartu Youth AcademyUppsala 10 51003 Tartu linn, Tartu linn, Tartumaa EST0Student Union OfficeÜlikooli 18b 51005 Tartu linn, Tartu linn, Tartumaa EST0Centre for Learning and TeachingArea of Vice Rector for ResearchUniversity of Tartu LibraryW. Struve 1 50091 Tartu linn, Tartu linn, Tartumaa EST0Grant Office
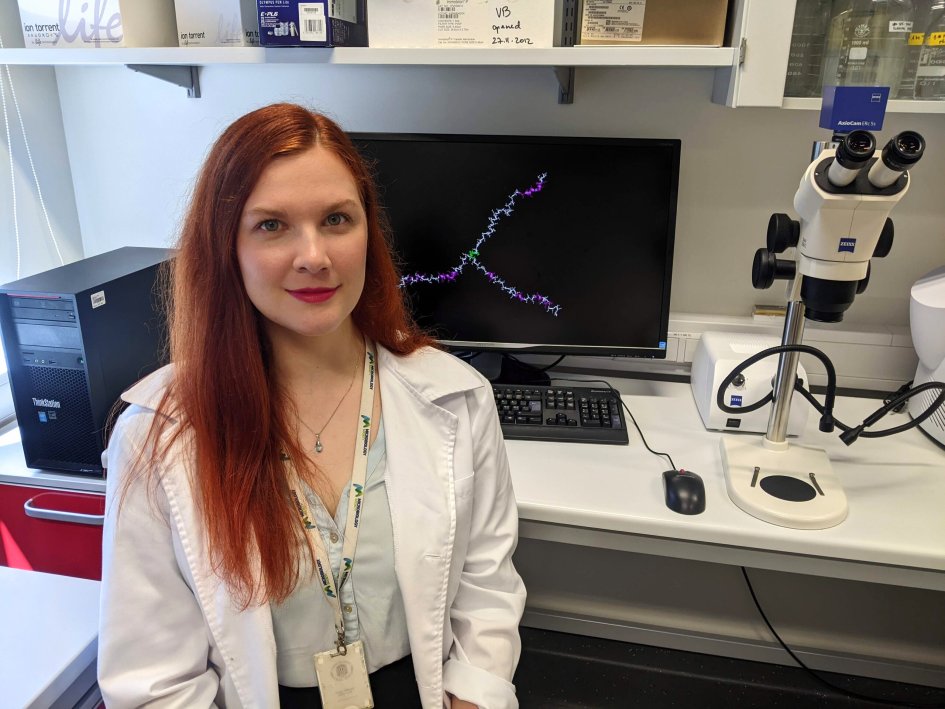
New drug suggests more successful breast cancer treatment in future

University of Tartu researchers in cooperation with colleagues from the Principe Felice Research Center of Valencia, Spain have developed a new drug called OximUNO, which has shown to treat breast cancer in mice. The first successful trials showed that OximUNO may in future effectively treat the most aggressive type of breast cancer. The results have been published in Cancer Research Communications, a journal of the American Association for Cancer Research (AACR).
Anni Lepland, doctoral student of biomedicine and translational medicine of the University of Tartu, led by Dr. Pablo Scodeller (associate professor of UT) and Prof. Tambet Teesalu (head of the Laboratory of Precision and Nanomedicine), has together with the spanish colleagues developed a drug for triple-negative breast cancer. “This is the most aggressive type of breast cancer and the most difficult to cure. The treatment options are therefore quite limited. The problem is that in the course of therapy, also other cells of the body are affected, with potentially devastating consequences,” Lepland said.
Anni Lepland explained further that a tumor creates around itself an environment in which various cells live, including macrophages. “Under normal conditions, macrophages help us eliminate pathogens or heal wounds. However, macrophages are plastic or easily changeable by nature, and tumours take advantage of that. Cancer turns macrophages into bad, tumour-promoting cells and makes them work against the human,” Lepland explained.
Researchers have worked out a method that can distinguish between the so-called good and bad macrophages in the tumour environment and destroy the bad macrophages. Specifically, Anni Lepland’s supervisors Dr Pablo Scodeller and Professor Tambet Teesalu developed a peptide or amino acid chain that is able to find the bad macrophages. “The peptide helps the OximUNO drug to find and bind to bad macrophages, and thereby deliver the drug into the cell, eventually destroying the cell,” Lepland said.
The researchers carried out three treatment trials and one survival study in mice, showing that treatment with OximUNO reduces primary tumour lesions and lung metastasis, and prolongs the survival of mice with triple-negative breast cancer. “Two treatment trials studied how the administration of OximUNO affects the size of the tumour in breast tissue. The results showed that the tumour in the breast tissue decreased in size, and OximUNO was also found to be able to reduce self-induced lung metastases. This was the reason for the decision to continue to study OximUNO’s effect specifically on lung metastasis,” Lepland explained. Experiments confirmed that OximUNO was able to reduce the size and the amount of tumor nodules in the lung.
Finally, a survival study was conducted, showing that OximUNO could extend the survival of mice. Therefore, the work allows to conclude that OximUNO reduces the tumour in the breast tissue, prolongs survival rate and can curb lung metastasis. “The latter is a very important aspect as metastases make cancer treatment more difficult. If cancer has spread to various parts of the body, the treatment options are even more limited,” Lepland added.
According to Lepland, the experiments showed OximUNO to be safe and effective, precisely targeting the bad, tumour-associated macrophages. The drug was also shown not to endanger other cells of the body.
There are many companies and different clinical trials that target tumour-associated macrophages in cancer treatment. Work is also underway to combine the treatment of tumour-associated macrophages with other treatment methods.
Anni Lepland said that it can take 10–15 years from a discovery to clinical trials. “Although we showed that OximUNO has an impact on the development of tumour, we did not cure the mice. Before we can move on to human trials, we need more solid results. When the drug makes it into human trials, its inclusion in actual tumour treatment will depend on whether or not it works in humans.”
Anni Lepland’s supervisors are Dr Pablo Scodeller and Professor Tambet Teesalu of the University of Tartu Laboratory of Precision and Nanomedicine. For the project, they mainly cooperated with the laboratory of Dr. María J. Vicent at the Principe Felipe Research Center of Valencia and with Dr. Alessio Malfanti of Université Catholique de Louvain. The work is mainly funded by Pablo Scodeller’s ETAg grant received in 2018.
Read more similar news






